How to Choose the Correct Blood Type - Part 1
As a new physician at Carter BloodCare, I am learning all about our specialty services – what kind of services we offer and how we meet the needs of both our local and remote healthcare communities. We offer expertise in many fields of transfusion medicine/blood banking. It is really a blood banker’s dream job!
As I embark on this journey, I would like to share my experiences with you. The world of transfusion medicine is growing and it is imperative to change and grow in order to keep up with the needs of our patients – both near and far.
How to choose the correct ABO blood type?
My first order of business is to explain what many might think is a basic question in the world of blood banking – How do I choose the correct ABO blood type for my patient? While it has become second nature to me over time, I remember having to work to understand these concepts as a medical student – it’s not as easy as one would like to believe.
In order to understand what type of blood is right for your patient, I like to separate it into 2 main types of blood products; red and yellow products. This is an important distinction because we are concerned about different types of compatibilities with each of these respective types of blood products. An incompatible “red product” is referred to as major incompatibility and an incompatible “yellow product” is referred to as minor incompatibility. And there is a very important, clinically significant reason for this distinction.
Selecting the right “red product”:
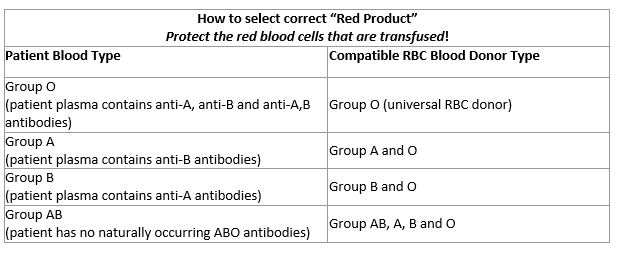
The most commonly transfused “red product” is packed red blood cells. There are other “red products” which we only transfuse in certain situations – granulocytes and whole blood. Basically, a “red product” is any product which contains ≥2mL of RBCs (and therefore must be crossmatched prior to transfusion). It is essential to transfuse ABO compatible red blood cells to a patient, because getting this wrong can be deadly – and is a hospital sentinel event.It was explained to me early on in my training, that, in blood banking, we must protect the red blood cells that are transfused! Therefore, the donor RBCs must lack any of the ABO antigens that the patient is also lacking, because the patient has naturally occurring antibodies against whichever ABO antigens (A or B) are lacking on their RBCs. This is why type O blood (no ABO antigens) is the universal “red product” and why type AB blood is the most restrictive “red product.” Of note, whole blood must be either type-specific or low titer group O whole blood, as both the red blood cells and plasma in the product must be compatible with the patient.
Selecting the right “yellow product”:
Because of the presence of naturally occurring ABO antibodies, yellow product compatibility is opposite to RBC compatibility. An incompatible yellow product (minor incompatibility) occurs when the naturally occurring ABO antibodies present in donor plasma react with either A or B antigens on patients’ red blood cells. While this is technically an incompatible product, it is less clinically significant. Minor incompatible products can potentially cause hemolysis of patient’s RBCs, but this is an uncommon occurrence. In fact, plasma is the only yellow product which should be compatible with a patient’s ABO type - platelets and cryoprecipitate do not. However, our AABB Standards for Blood Banks and Transfusion Services (our accreditation requirements) does have some safety regulations regarding transfusing incompatible yellow products. It says that a transfusion service must have a process in place in order to avoid transfusing significant amounts of plasma containing incompatible ABO antibodies to patients (5.15.4). And this is an important safety guideline – as there are (albeit rare) case reports of patient harm due to receiving too much incompatible plasma.
Check back next week for Part 2 of this blog on “How To Choose the Right Rh Blood Type.”
References:
Standard for Blood Banks and Transfusion Services, 32nd ed. April 1, 2020.
AABB Technical Manual, 19th ed. 2017. Edited by Fung M, Eder AF, Spitalnik SL and Westhoff CM.